Monday, May 31, 2021
Sunday, May 30, 2021
World No Tobacco Day
Saturday, May 29, 2021
Cancer prevention & early detection still suboptimal in the U.S.
Historical gains in smoking cessation undercut by social and geographic disparities.
Cancer prevention and early detection measures show mixed progress, and substantial racial/ethnic, socioeconomic, and geographic disparities continue to exist, according to American Cancer Society data on cancer prevention and early detection efforts in the U.S. in 2018 and 2019, pre-COVID-19.

This study is published in Cancer Epidemiology, Biomarkers & Prevention, a journal of the American Association for Cancer Research, and accompanies our biennial report, Cancer Prevention & Early Detection Facts & Figures (pictured above). It is one of the only sources that looks at major modifiable cancer risk factors, including tobacco use, obesity, diet and physical activity, HPV vaccination, ultraviolet radiation exposure, environmental exposure, and screening test use.
In 2021, an estimated 608,570 cancer deaths are expected to occur in the U.S. with about 45% attributable to behaviors that could be changed, such as cigarette smoking, excess body weight, alcohol intake, physical inactivity, and unhealthy diet. Cigarette smoking alone accounts for nearly 30% of cancer deaths.
The article, led by Priti Bandi, PhD (pictured here), reported a mixed picture, with historic lows in smoking rates but suboptimal obesity, cancer screening, and HPV vaccination levels. Additionally, racial/ethnic, and socioeconomic status disparities persisted across most major modifiable cancer risk factors and preventive outcomes. We know that screening rates, not where we wanted them to be pre-COVID, dropped precipitously during the pandemic.
Tobacco
Cigarette smoking in 2019 reached a historic low (14.2%) mainly because 61.7% (54.9 million) of all persons who ever smoked quit (a measure also known as the quit ratio). While the quit ratio has improved across most subpopulations since 1965, it continues to be lower among persons who are Black, American Indian/Alaska Native, poor, lower educated, lesbian, gay, or bisexual, and residents of Southern states.
Persons who smoke in many of these same subgroups also have lower levels of recent successful cessation, despite having similar or higher quit attempt levels. This disparity was most striking among lower-income and Medicaid insured or uninsured persons in whom the successful cessation rate is about 40% lower than higher income and privately insured persons, respectively, even though their quit attempt prevalence was similar.
Despite being recommended as effective clinical cessation interventions since the late-1990s, only 71.7% reported getting medical doctor advice to quit, and just about 1 in 3 used evidence-based cessation treatments for tobacco dependence in 2018-2019, with significantly lower levels among those who were Hispanic, younger, and Southern residents.
“While historical gains in smoking cessation have led to steep declines in lung cancer mortality in the past decade, substantial progress can still be made by improving cessation outcomes among socially vulnerable groups. Much can be achieved by expanding tobacco cessation coverage in state Medicaid programs and equitably implementing effective tobacco control policies within and across U.S. states,” Dr. Bandi said.
Cancer Screening
Early detection of cancer through screening reduces mortality from cancers of the breast, cervix, colon, rectum, and lung. Colorectal and cervical cancers screening can also prevent these cancers by identifying precancerous lesions that can be removed. Cancer screening prevalence was suboptimal in 2018 (colorectal cancer ≥50 years: 65.6%; breast ≥45 years: 63.2%; cervical 21-65 years: 83.7%), especially among uninsured adults (colorectal: 29.8%; breast: 31.1%).
Approximately 18% of cancer cases in the U.S. can be attributed to a combination of excess body weight, insufficient physical activity, unhealthy diet, and consumption of alcoholic beverages.
Excess Body Weight
Obesity levels remain high in 2017-2018. Among adults >20 years, the prevalence of obesity was 42.4% (an estimated 99.14 million adults), and the prevalence of overweight was 30.7%. Overall, obesity prevalence was disproportionately higher among Black (56.9%) and Hispanic (43.7%) women and lowest among Asian men (17.5%) and women (17.2%).
Physical Activity
In 2018, over a quarter (25.6%) of adults reported no leisure time physical activity. The disparity by education was vast, ranging from nearly half (48.2%) of people with <high school education compared to 14.5% of college graduates.
Diet
Overall, most adults do not meet the guidelines for healthy eating. In 2019, about 12.3% of adults reported consuming three or more servings of vegetables per day and about 26.2% of adults reported eating two or more servings of fruit daily. Vegetable consumption was higher among Asian and White women than Hispanic or Black women.
Alcohol
In 2018, an estimated 5.1% of adults were classified as heavier drinkers (12+ drinks in lifetime, and >14 drinks per week for men; >7 drinks per week for women). Heavier alcohol consumption increased with higher levels of education among women (2.4% with less than a high school diploma vs. 6.4% of college graduates); whereas among men prevalence was highest (7.1%) in men with less than a high school diploma and lowest (4.2%) among college educated.
HPV Vaccination
In 2019, data show the HPV vaccination in adolescents (aged 13-17 years) remains underutilized and over 40% were not up to date. In adults (ages 19-26 years), 52% of women and 31.7% of men reported ever having received one or more dose of the HPV vaccine.
“More work is needed in order to further reduce cancer risk factors and improve cancer screening,” said the authors. “Immediate actions are needed to increase smoking cessation in health disparate populations, stem the tide of obesity epidemic, and improve screening and HPV vaccination coverage.”
*Shared from MySocietySource.
Assets available to help ACS urge the public to ‘Get Screened’
Get Screened and I Got Screened Facebook profile frames now available!
You already know that a big part of our mission work this year is focused on increasing cancer screening rates. Today, we're taking another big step forward in this effort by launching our Get Screened public awareness campaign.
The public screening campaign is one of six components of our effort to make sure people are getting their recommended cancer screening tests. Read this My Society Source story for a look at the big picture.
ACS's promotional campaign
ACS's campaign will focus on a combination of earned and paid media. Our paid media campaign centers around digital media, specifically Facebook and Instagram. The campaign launches this summer and will run through October.
New landing page on cancer.org
The campaign has a new landing page on cancer.org. The page addresses how to overcome barriers to cancer screening, including what to do if someone is uninsured or underinsured. More information is available about the ACS guidelines for cancer screening. The landing page is available at cancer.org/get-screened.
Asset overview and availability
Available is a list of screening educational materials that you can download and use with partners, volunteers, and the public. We also have a social media profile picture frames available on Facebook, so show your personal support for the campaign by adding the Get Screened or I Got Screened frame to your profile pic. To add a frame, open Facebook, navigate to your profile, and click on your profile pic. Select ‘add frame’ and search ‘American Cancer Society’ to find the Get Screened frame.
Call to action for volunteers
- If you're not up to date on screening, call your doctor.
- Share and re-post the American Cancer Society's screening social media messages when you see them. Remember to use the campaign hashtag – #GetScreened – in all your posts.
- Show your support for the campaign on Facebook by adding our Get Screened social media profile picture frame to your Facebook profile pic. To add the frame, open Facebook, navigate to your profile, and click on your profile pic. Select 'add frame' and search 'American Cancer Society' to find the Get Screened frame.
- Learn more by visiting our new landing page at cancer.org/get-screened.
- Talk to your staff partner about how you can get involved in our local efforts to get cancer screening rates back on track.
Report on cancer research and disparities
Non-Whites more likely to report negative experience about their treatment.
A new report from the American Cancer Society Cancer Action Network (ACS CAN) takes an in-depth look at disparities across all areas of cancer research and suggests immediate policy solutions that could help address such gaps in the years to come.

The report, Cancer Research and Disparities: Understanding and Addressing the Issues, finds that different types of research can either exacerbate or minimize cancer disparities, as can the makeup of the cancer care and research workforce.
For instance, while racial and ethnic minority groups and older patients are equally willing to participate in clinical trials as other groups, they are often underrepresented in clinical trials. Reasons for this disparity include everything from insurance status and trial location to the trial designs themselves, which often do not identify, understand, or address disparities in cancer outcomes.
Also, research to identify and address disparities in outcomes has to be deliberate and specifically designed. This research often requires significant over-representation of certain populations and the inclusion of information from a wide array of clinical and social science work. Without such an approach, research may miss why cancer outcomes are often worse for patients with limited access to care, lower socioeconomic status, and other factors.
“Addressing disparities in all areas of cancer research is essential to tackling the disproportionate cancer burden communities of color and people living in under-resourced areas too often experience,” said Lisa Lacasse, president of ACS CAN. “No one should be disadvantaged in their fight against cancer because of how much money they make, the color of their skin, their sexual orientation, their gender identity, their disability status, or where they live.”
Yet preliminary results from a forthcoming ACS CAN Survivor Views survey, finds Hispanic and non-white respondents were more likely to report a negative experience when asked about different aspects of their treatment, including whether they were confident they had access to the best and most effective treatment, if they were an active participant in their care, and whether they were able to get the preventive care needed as a survivor. And more than 1 in 8 respondents whose annual household income is $35,000 or less reported that it is not easy to receive preventive care like check-ups and regular cancer screening.
Policy measures that would address research disparities were discussed during ACS CAN’s National Policy Forum on the Future of Health Care earlier this month and were included in the report:
- Shield patients from out-of-pocket ancillary costs of trial participation: The U.S. Department of Health and Human Services' Office of the Inspector General should clarify policies to ensure reimbursement of ancillary costs such as travel, parking, and housing by clinical trial sponsors is not seen as undue influence and ensure awareness of allowable reimbursements.
- Maintain and expand access to Medicaid: State Medicaid programs provide essential coverage for people with limited incomes including various populations likely to be underrepresented in clinical trials.
- Issue permanent guidance on the conduct of decentralized clinical trials: During the COVID-19 pandemic the U.S. Food and Drug Administration (FDA) significantly expanded opportunities for the use of decentralized trial practices like telemedicine, which could allow greater participation of underrepresented groups in clinical trials. These flexibilities are set to expire with the end of the public health emergency.
- Address genetic variation leading to disparate responses to cancer therapeutics: Ancestry and genetic inheritance can have a direct effect on how a drug is metabolized, thus affecting the safety and efficacy of the treatment. FDA should collect evidence regarding differential safety and efficacy of therapies based on ancestry and ensure drug labeling accurately reflects these differences. Congress could also give FDA the authority to require sponsors to design clinical trials with appropriate demographic representation when prior evidence points to likely ancestral disparities in safety or efficacy.
- Invest in a diverse cancer care and research workforce: The National Institutes of Health (NIH), the National Institute on Minority Health and Health Disparities (NIMHD), and the National Cancer Institute (NCI) should expand existing opportunities and programs that support career development for scientists and researchers from underrepresented minority groups.
“Cancer research needs to reflect the people and communities it is meant to serve,” said Lisa. “We cannot afford to ignore or neglect the critical role of diversity in advancing medical science. We need to take decisive action to eliminate cancer disparities in all areas of cancer care, including in cancer research.”
*Shared from MySocietySource.
Friday, May 28, 2021
National Sunscreen Day
Wednesday, May 26, 2021
ACS CAN to President & Congress: Make affordable health care a priority
Before his address to a joint session of Congress, the American Cancer Society Cancer Action Network (ACS CAN) urged President Biden and Congress to work together to prioritize access to affordable health care in any forthcoming infrastructure legislation.
ACS CAN sent a letter to the White House and Congressional leadership ahead of the president’s address to Congress detailing several policies that would help more Americans prevent, detect, and treat cancer successfully.
The letter calls for:
- Making permanent the expanded eligibility and generosity of subsidies to cover the costs of marketplace health plans—policies that have contributed to more than a half million people gaining health care coverage in just a few months—fixing the “family glitch” so that families are able to afford coverage through the marketplace if someone's employer only offers affordable coverage for the employee
- Continuing to expand coverage to low-income populations
- Prohibiting or significantly curtailing the sale of substandard insurance plans, including short-term limited-duration plans, association health plans and farm bureau plans, all of which are exempt from covering the kind of services those with cancer or a history of cancer need
- Capping out-of-pocket drug costs for people in Medicare Part D
A statement from ACS CAN President Lisa Lacasse follows:
“The president and Congress have a unique opportunity to make permanent changes that have made health care more affordable and accessible during this pandemic and extend the benefits of improved access to cancer prevention, detection and treatment services for millions of American for years to come. Combined, expanded eligibility and generosity of health care subsidies, including ending the family glitch, expanding coverage to more low-income individuals, and reigning in substandard insurance plans would vastly improve the country’s access to comprehensive health care. Research has repeatedly shown the connection between adequate health coverage and early cancer detection and survivability.
“With no current limit on out-of-pocket costs for prescription drugs in Medicare, cancer patients can face staggering costs to access recommended treatments. Capping out-of-pocket drug costs for Medicare enrollees would alleviate the often-overwhelming financial burden cancer patients face that can create barriers to timely and lifesaving treatment.
“The coronavirus pandemic has made clear the nation’s urgent need for more affordable, comprehensive health care coverage and provides an opportunity for lawmakers to meet that need now and in the future. On behalf of cancer patients, survivors and their families we urge the president and Congress to make access to affordable health care a policy priority in their upcoming infrastructure bill.”
*Shared from MySocietySource.
Tuesday, May 25, 2021
ACS urges parents to get their kids vaccinated against HPV now
Before they become eligible for COVID-19 vaccinations.
Each summer, ACS reminds parents to talk to their children’s health care providers about preventing six types of cancer via HPV vaccination. This year, our campaign is launching earlier, and with more urgency than ever, for two important reasons.

First, the COVID-19 pandemic has resulted in a decline in vaccination rates as parents canceled pediatrician visits to avoid being exposed to the virus. As a result, the CDC estimates that HPV vaccinations are down by more than 20% – or 1 million doses – compared to 2019.
Second, experts predict the COVID-19 vaccination will be available to adolescents at some point this summer. If that’s the case, children who get the COVID-19 vaccine will have a seven- to eight-week window in which they cannot receive any other vaccinations, spanning the time before, during, and after they receive the COVID-19 vaccination.
What ACS is doing
It’s clear that now is the time to get children caught up on routine immunizations they might have missed during the pandemic and before COVID-19 vaccination is available to that age group.
In response, ACS is using a combination of earned and paid media starting May 3 and continuing through late August to encourage parents to talk to their children’s doctors about HPV vaccination.
Our target audience includes:
- Parents/guardians of children age 9-12. In general, people ages 38-50.
- Parents, with a focus on moms as the family health decision makers.
- People of are unaware or lack of knowledge about the HPV vaccine and who may be hesitant or cautious.
- Parents living in communities with lower vaccination rates
Why it matters
HPV vaccination helps protect against 6 types of cancer. It helps protect boys from cancers of the throat, penis, and anus later in life and helps protect girls from cancers of the cervix, throat, vagina, vulva, and anus later in life. Vaccination can prevent more than 90% of HPV cancers when given at the recommended ages.
It works best when given between ages 9-12, though children and young adults ages 13-26 can and should receive the vaccine if they are not up to date.
Vaccination is for girls and boys, and it’s been proven safe, effective, and long-lasting.
More than 60% of parents in the U.S. have chosen to protect their children from HPV cancers. ACS’s Mission: HPV Cancer Free campaign aims to boost that number to 80% by 2026.
Action for volunteers
If you’re the parent of a child age 9-12, talk to your pediatrician about making sure your child is protected from HPV cancers.
For more about our HPV efforts, visit cancer.org/hpv. And for information about getting vaccinations during the pandemic, visit cancer.org/covidandhpvvaccine.
*Shared from MySocietySource.
Monday, May 24, 2021
Sunday, May 23, 2021
Watch the replay of ACS CAN's health equity chat
Speakers include Rep. Lisa Blunt Rochester and ACS CAN Board Member and The Links, Inc. President Kimberly Jeffries Leonard.
The American Cancer Society Cancer Action Network (ACS CAN) hosted a virtual volunteer engagement event on April 27 at 7 p.m. ET featuring U.S. Representative Lisa Blunt Rochester (D-DE) and Dr. Kimberly Jeffries Leonard, ACS CAN Board Member and National President of The Links, Inc. Watch the replay.
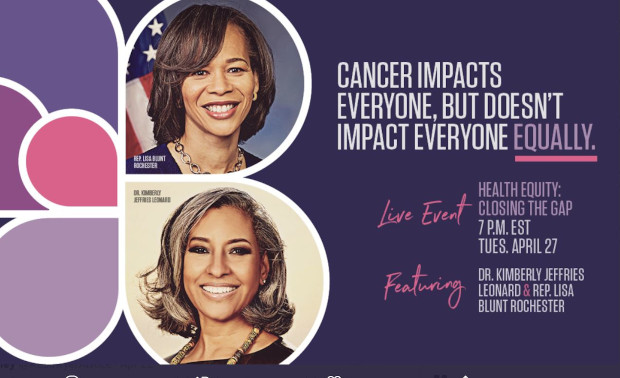
Moderated by ACS CAN Federal Relations Director Illy Jaffer, the event, Health Equity: Closing the Gap, focused on addressing health disparities and advancing health equity. A member of the Congressional Black Caucus, Rep. Blunt Rochester discussed the Quit Because of COVID-19 Act ( H.R. 2185), legislation she introduced to increase tobacco cessation services in Medicaid. She also shared additional health equity work she’s doing. Dr. Jeffries Leonard discussed ACS CAN’s efforts to increase health equity as well as those of The Links, Inc.
The event aired live on ACS CAN’s Facebook page.
ACS CAN is committed to partnering with lawmakers, civic leaders, and other organizations to make sure everyone has the same opportunity to prevent, treat, and survive cancer. To learn more about our health equity work, visit fightcancer.org.
*Shared from MySocietySource.










