Report shows milestone advances in lung cancer early detection and survival.
There’s major progress in the fight against lung cancer. Although lung cancer continues to be the leading cause of cancer death, patients are finally being diagnosed earlier and living longer. This was one of the major findings in Cancer Statistics, 2022, the latest edition of the American Cancer Society’s annual report on cancer rates and trends released Wednesday, Jan. 12, 2022.
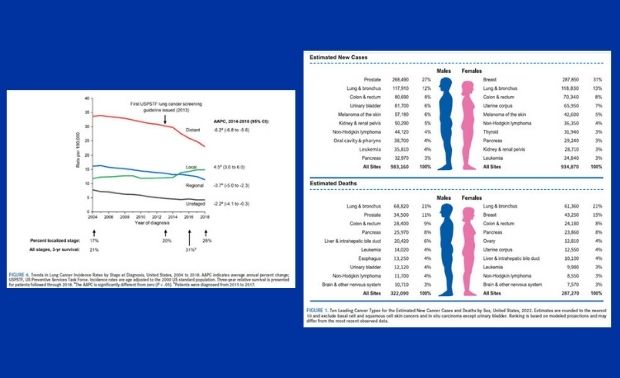
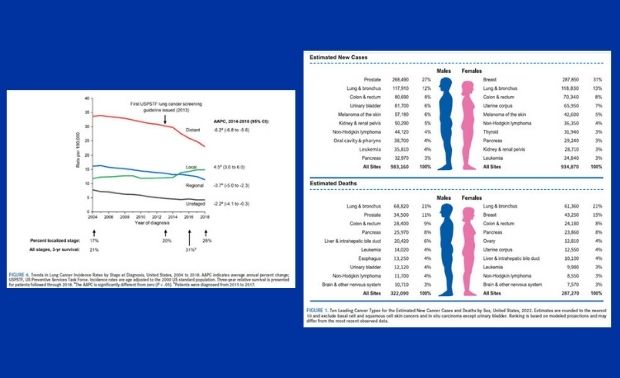
According to the report, 28% of lung cancers in 2018 were detected at a localized stage of disease vs just 17% in 2004. People are also living longer with 31% of patients surviving 3-years after diagnosis compared to only 21% a decade ago. Experts at the American Cancer Society credit these milestone advances to increased access to care (through the Affordable Care Act) and lung cancer screening, as well as improved treatments.
Lung cancer causes the most deaths of any cancer by far – 350 per day – more than breast, prostate, and pancreatic cancers combined. While 80% of lung cancer deaths can be attributed to smoking, there will be an estimated 20,700 deaths from lung cancer in 2022 that are not related to smoking. That would rank nonsmoking related lung cancer as the eighth leading cause of cancer death among sexes combined if it was classified separately.
Steep declines in lung cancer mortality helped spur an acceleration in the pace of decline in overall cancer mortality, from about 1% per year during the late 1990s to 1.5% per year during the 2000s and 2% per year from 2015 through 2019. This progress is alongside slowing reductions in mortality from other leading causes of death like heart diseases. The 5-year relative survival rate for all cancers combined increased to 68%, up from 49% in the mid-1970s.

Overall, there will be an estimated 1.9 million (1,918,030) new cancer diagnoses and 609,360 cancer deaths in the United States in 2022. These estimates do not reflect the impact of COVID-19 because they are based on currently available incidence and mortality data through 2018 and 2019, respectively. The lifetime probability of being diagnosed with invasive cancer is slightly higher for men at 40.2% than for women at 38.5%.
While there is plenty of positive news, there are also many areas of concern. For example, cervical cancer is almost completely preventable, yet more than 10 women die from the disease each day in the US, half of whom are in their 50’s or younger.
“Despite an accelerating drop in cancer mortality overall, including exciting recent advances against lung cancer, it’s frustrating to still see thousands of preventable deaths each year from cervical cancer,” said Rebecca Siegel, MPH, Senior Scientific Director of Surveillance Research at the American Cancer Society and the lead author of the report. “Most of these women have never been screened, so this is low-hanging fruit easily addressed by increasing access to screening and vaccination among underserved women.”
Researchers are watching prostate cancer closely. Although prostate cancer incidence is stable overall, the rate of advanced-stage disease diagnosis increased by 4%-6% annually from 2014 through 2018, likely reflecting declines in the use of PSA testing. The value of screening is especially salient for Black men, who have had a steeper drop in PSA testing than White men despite two-fold higher prostate cancer mortality.
Researchers also noted the continued rise in female breast cancer incidence, which has been slowly increasing by about 0.5% per year since the mid-2000s. This is attributed, at least in part, to continued declines in the fertility rate and increases in excess body weight which are both known risk factors. The rising incidence for breast and advanced stage prostate cancers, both of which can be detected early, is concerning, the report notes.
Even more alarming, according to the report, is the persistent racial, socioeconomic, and geographic disparities for highly preventable cancers. These disparities typically develop and/or are exacerbated by uneven access to interventions such as screening, HPV vaccination, and treatment advances. The report concludes increased investment in the broad application of existing cancer control interventions and basic and clinical research to further knowledge and advance treatment options would undoubtedly accelerate progress against cancer and mitigate racial and socioeconomic inequalities.
*Shared from MySocietySource.